The Hippocratic Oath, a time-honored pledge among physicians, extends beyond the commitment to “first do no harm.” Its essence, encapsulated in the Latin phrase “primum non nocere,” underscores the ethical foundation of medical practice, emphasizing the imperative to avoid harm and reject intentional wrongdoing.
However, this principle has recently been appropriated by some anti-vaccine advocates, including individuals who profess to be medical professionals or biomedical scientists. Concerns regarding vaccine safety and efficacy are not new; they predate the COVID pandemic, harking back to discredited claims that linked vaccines for measles, mumps, and rubella to autism. Alarmingly, a national survey has found that 12% of Americans now believe that mRNA COVID vaccines could cause cancer, a notable increase from 9% a year earlier.
This growing skepticism is exacerbated by reports of adverse vaccine reactions, particularly severe allergic responses associated with COVID vaccinations, which further fuel public hesitance. Such doubts could impede vaccination rates, potentially increasing the risk of serious illness and mortality and threatening public health, especially as disease outbreaks loom.
Recent public opinion surveys reveal a concerning trend regarding public confidence in vaccinations:
• Only 63% of respondents believe that the COVID vaccine is safer than the virus itself, down from 75% in April 2021.
• The percentage of individuals attributing rising autism cases to increased vaccine administration has climbed from 10% to 16%.
• While 67% of people report a return to pre-pandemic normalcy, 75% indicate that they rarely or never wear face masks.
• Over 10% of respondents suspect vaccines contain toxic ingredients, up from 8%.
• Nine percent erroneously think flu shots increase the risk of COVID, up from 6% in earlier surveys.
• Only half of respondents agree that the seasonal flu vaccine does not cause the flu.
Despite warnings from pro-vaccine advocates that unvaccinated adults accounted for an estimated 232,000 vaccine-preventable COVID-related deaths in the U.S. from May 2021 to September 2022, resistance to vaccination remains strong. Further complicating matters, cardiovascular complications associated with SARS-CoV-2 infection are common, leading to significant morbidity in chronic cases that affect quality of life and health outcomes. According to the National Institutes of Health (NIH), individuals recovering from COVID may face an increased risk of myocarditis, dysrhythmia, pericarditis, ischemic heart disease, heart failure, and thromboembolism.
Key points from NIH underscore the urgency:
• Cardiovascular complications are prevalent following acute and post-acute COVID infection.
• The underlying biological mechanisms remain poorly understood and complex.
• No singular treatment has been identified for post-COVID cardiovascular disease; thus, established guidelines for specific cardiovascular conditions should be followed.
• Cardiac rehabilitation is recommended for eligible individuals.
In this context, the digital realm—especially social media—has added layers of complexity, serving as both a platform for accurate information and a hotbed for misinformation about vaccines.
The latest statistics from the Centers for Disease Control and Prevention (CDC) reveal an 18.1% COVID test positivity rate as of the week ending August 10, 2024, marking the highest level since January 2022. Concurrently, wastewater surveillance data indicates “very high” levels of viral activity nationwide, suggesting that real positivity rates may be even higher.
As respiratory virus season approaches, the Department of Health and Human Services has initiated a public education campaign focused on common respiratory illnesses and the vaccines available for flu, COVID, and respiratory syncytial virus (RSV). The CDC now recommends that everyone aged six months and older receive an updated COVID vaccine for the 2024-2025 season, with a particular emphasis on booster shots for seniors aged 65 and older due to emerging new variants.
While an impressive 93% of seniors have received at least two doses of the COVID vaccine, compliance among healthcare professionals is surprisingly low. Given the substantial medical literature underscoring the efficacy and safety of vaccines, these numbers should raise alarms. Healthcare workers, having seen firsthand the benefits of vaccination—like reduced symptom severity in vaccinated patients—must urgently advocate for these preventive measures.
To shift the culture of vaccination from hesitation to acceptance, healthcare providers must emerge as credible advocates. With the risk of rising infection rates during holiday and travel seasons, the stakes could not be higher—the health of our communities hangs in the balance.
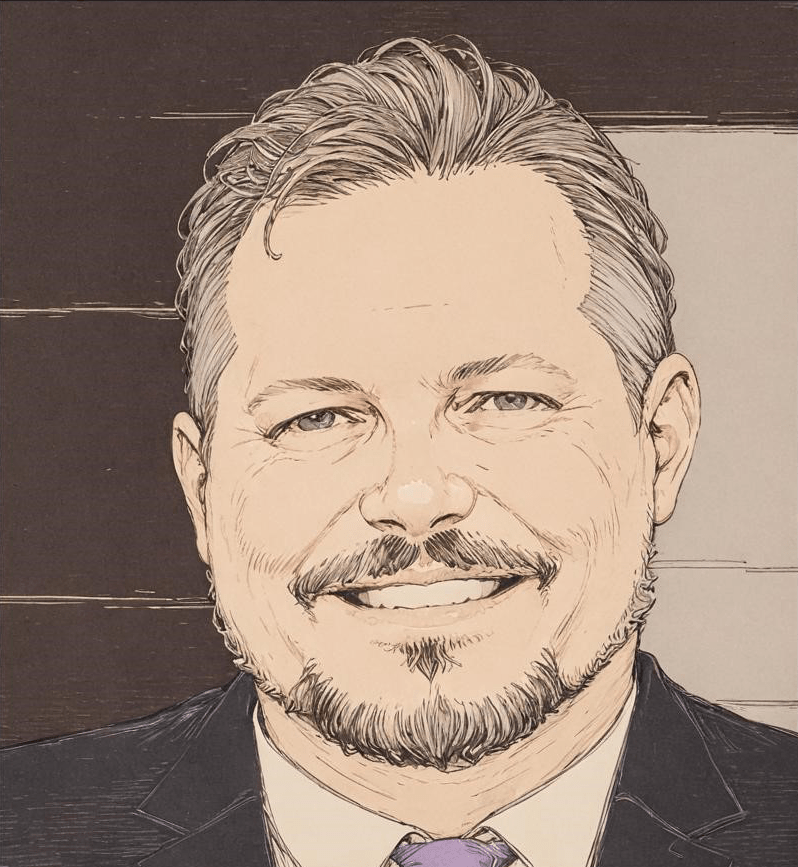
Russell R. Barksdale, Jr., PhD., MPA/MHA, FACHE is President and CEO of Waveny LifeCare Network